*Disclaimer: The following should not be misconstrued as medical advice. Discuss medical issues with your physician. Joe Bender and The Bender Observatory are wholly independent and are not affiliated with any of the cited sources of this information. Joe Bender and The Bender Observatory are not associated with the pharmaceutical cartel, the big-pharma-controlled American Medical Association [AMA], the tax-exempt globalist foundations, or the state-controlled American mainstream media.
Introduction
“It is indeed difficult to persuade some to practice, when in health, what is necessary to preserve so valuable a blessing.”
-Dr. James Lind, A Treatise of the Scurvy, 1753
“We believe that the development of sustainable health paradigms of tomorrow will require a multidisciplinary approach today. This approach will, at times, require each of us to look to the literature found in diverse fields of endeavor, for better understanding, particularly in areas in which we were not formally trained.”
-Dr. Stephanie Seneff and Dr. Robert M. Davidson, The Initial Common Pathway of Inflammation, Disease, and Sudden Death, 2012
“We live on an island surrounded by a sea of ignorance. As our island of knowledge grows, so does the shore of our ignorance.”
― Dr. John Archibald Wheeler, 1992
Healthy blood circulation, after good relationships with God and our families, is the most important thing I can think of, because without it we can’t live. Cardiovascular disease is far too common, and the underlying causes need more research, to help treatment shift from the poor approach of alleviating symptoms, to the desirable approach of correcting the underlying problems. I shared the first quote above because I sometimes struggle to stay vigilant in addressing health factors, and I hope to encourage others to recognize the value of their health, and to alert them to ways they can maintain or improve it. The latter two above quotes outline issues in our modern approach to scientific endeavors, and the importance of keeping an open mind to increase our understanding. This paper is a collection of potentially helpful elements involved in cardiovascular health, and underscores promising areas that need more research.
Key Takeaways:
Staying well-hydrated helps blood flow by keeping it from being too ‘thick.’
Movement throughout the day is needed to squeeze blood back to the heart by the action of muscles and one-way valves throughout the veins.
Most people consume too much omega-6 and not enough omega-3.
Heart disease may be a result of a low-level chronic deficiency of vitamin C (ie subclinical scurvy).
B vitamins are important for cardiovascular health and are involved in dilation of blood vessels.
Nitric oxide is a key signaling molecule for the entire vascular system, and is involved in blood vessel dilation.
Dietary sulfur and sunlight exposure may be key factors in healthy circulation.
Emulsifiers/surfactants are hazardous to the cardiovascular system.
The Role of Hydration
The viscosity of our blood is largely determined by water content[1]. Viscosity is a measure of how flowable a liquid is. Tar, for example, has a much higher viscosity than olive oil. Drinking water and other fluids decreases blood viscosity, and is said to ‘hydrate’ our bodies, by increasing the water content in our cells, cerebrospinal fluid (the fluid that surrounds the brain and spinal cord), and bloodstreams. The ratio of red blood cells to the total volume of blood is called hematocrit. Hematocrit is decreased by hydration (ie there is more fluid relative to blood cells), allowing for better circulation by decreasing blood viscosity[2]. When we don’t drink enough fluids, the blood loses water content and flows less efficiently, and is more likely to clot.
A 2013 study published in Alternative Therapies studied the effects of hydration and exercise-induced dehydration on the whole blood viscosity [WBV] of firefighters, because cardiovascular disease is their number one cause of on-duty death, accounting for 45% of these deaths, and the working conditions firefighters experience make them prone to dehydration[3]. The study’s findings suggested a “profound influence of hydration states on WBV,” and the researchers concluded that the WBV of firefighters should be monitored as an important metric of cardiovascular health. The study participants had elevated WBV (ie thicker, more-viscous blood) associated with dehydration from exercise, and subsequent rehydration reduced their WBV.
Another study, by Song et al. (2017), from BMC Neurology, examined the role of blood viscosity in disease of small blood vessels in the brain[1]. The authors cited three previous studies indicating that elevated blood viscosity caused by dehydration is a key factor culpable in inducing clot-caused stroke. Additionally, their own study involved 63 stroke patients, and found elevated viscosity in the blood of stroke patients immediately after hospitalization, which decreased after hydration therapy, and was found to again be elevated in these patients in a follow-up examination five weeks later. Their data, and findings of other studies, indicated that high blood viscosity over time, associated with dehydration, is an underlying cause of stroke.
Heart attacks, blood clots, and thromboembolisms (blood clots that travel from their site of origin and lodge in another vessel), are also associated with increased blood viscosity, as discussed by Sloop et al (2020)[2]. These authors showed further evidence that hematocrit is a paramount factor in blood viscosity, and is associated with hydration.
According to the World Health Organization [WHO], cardiovascular disease is the number one cause of death worldwide, representing 32% of all deaths[4]. 85% of cardiovascular deaths result from heart attacks and strokes. How many of these deaths could be prevented simply by consistent hydration?
Staying hydrated is revealed by the aforementioned studies and statistics to be an upsettingly overlooked circulatory factor that likely affects countless lives. There are apparently no public service announcements informing citizens of it. I never heard it in school. Could this be attributable to the fact that there is no money to be made by the medical establishment by teaching medical students the cardiovascular importance of hydration? Sure doctors sometimes tell their patients to stay hydrated, but if they told people it could prevent heart attacks and strokes, it would be taken a lot more seriously. With all of civilization’s advances in medical understanding, it is remiss that the role of hydration in healthy blood circulation receives so little attention.
How Veins Work
As blood travels from the heart throughout the body via arteries, the larger arteries branch into smaller and smaller arteries, the smallest of which are called arterial capillaries[5]. The arterial capillaries deliver oxygen and nutrients to the cells of the body.
Image: Capillaries are the smallest blood vessels, and are responsible for delivering nutrients and removing wastes from cells. There are roughly 10 billion capillaries in the human body.
Capillaries are so small that red blood cells have to pass through them single-file. Pumping the blood through such small-diameter vessels causes enormous pressure loss; so, once blood has reached the cells, most of the pressure from the heart is diminished. As blood travels back along veins toward the heart and lungs, it needs assistance because of the lack of pressure. This assistance is supplied by the much larger volume of veins in the body relative to arteries, thereby reducing resistance, and also by one-way valves positioned along the veins[5].
Image: One-way valves in veins move blood back to the heart and lungs when muscles contract and squeeze the veins.
Thanks to these valves, when the muscles of the body squeeze the veins, the blood can only be squeezed in one direction—back to the heart and lungs. This squeezing action is why bed-ridden patients must be moved frequently, to help avoid pooling of blood and resulting bedsores.
There is a growing body of evidence that truck drivers, lawyers, and other people who spend much of their day sitting may have a higher risk of blood clots because of being stationary and lacking the movement necessary to squeeze the veins and move blood back to the heart and lungs[6]. Atler et al. (2015) found that sitting for extended periods was associated with harmful outcomes, in a review of the medical literature[7]. Frequently standing up and sitting back down, flexing the muscles throughout your legs, and occasionally walking around or otherwise getting five minutes of movement every hour, may prevent heart disease by increasing circulation[8].
Dr. Kieth Diaz recommends getting up and moving around every 30 minutes[9], based on a study he led, that tracked the daily movement patterns of about 8,000 people, and found a doubled risk of death in those participants who fell into the sedentary category[10]. Setting a timer on your phone or watch, to remind you to stand up and move may be helpful, at least until you’re in a good habit of doing so. I’m having trouble finding this source, but I read another doctor’s recommendation about fifteen years ago, saying it is very beneficial for circulation to simply stand up and sit back down every ten minutes.
If you stand in place for long periods, this also may not provide enough movement for healthy circulation, so make an effort to periodically use your leg muscles however you can. Stationary standing has been associated with increased arterial pressure in the legs, leg discomfort, varicose veins, and other symptoms of vascular disorder in the legs[11]. This makes sense because of the increased “head height” in leg veins, created in the standing position. Water pumps have a head height limit; that is, they are limited in the total height they are capable of pumping water, and within their range of their capability, the flow rate of their output decreases with increasing pumping height. This is because water pressure increases with depth, as exemplified by the increased pressure a scuba diver experiences at lower depths. This effect can be visualized as a column of water above the diver weighing down on them; likewise, in a pipe or vein, as the height of the fluid column increases, so does the downward force of gravity (ie water pressure). So, standing increases the back pressure in blood vessels as a result of the increased fluid column height in veins; this necessitates extra squeezing of the muscles to utilize the one-way valves in veins to move blood back to the heart. In fact, standing still for excessive durations can cause people to faint due to lack of circulation[12]. If you have to stand for a prolonged period, I suggest periodically ‘taking a lap’ if you can, or doing a few calf-raises and squats, etc.
Elevating your legs when sitting also helps increase circulation, by decreasing the height of your heart relative to the position of your feet[13]. This can also reduce swelling of the legs and feet, decrease the incidence of veinal diseases, and reduce the chance of developing blood clots.
Exercising for at least 30 minutes daily is also important for heart health, but is not a substitute for frequent movement throughout the day, as found by the aforementioned studies[14]. Exercise, including swimming, walking, and strength training, increase the strength of the heart muscles, thereby aiding circulation[14]. Exercise also increases muscle mass throughout the body, resulting in elevated metabolism at rest, thereby benefiting cardiovascular health by decreasing body fat, and perhaps also by accelerating chemical reactions in cells that regulate the constriction and relaxation/dilation of blood vessels to control blood flow[15]. Body fat content regulates bloodstream cholesterol levels, and low HDL (‘good’ cholesterol) is associated with central (abdominal) body fat[87]. Therefore, decreased body fat from exercise may improve cholesterol status for healthier cardiovascular function. I’ll mention more about the chemical control of circulation below, in the sections on vitamin C, nitric oxide, b-vitamins, and Dr. Seneff’s novel hypothesis involving sulfur compounds and sunlight. So, for these and other reasons, exercise is important for cardiovascular health; but because a lack of movement throughout the day stifles blood flow driven by the one-way valves in veins, prolonged sitting or standing should be avoided, by periodically interjecting movements such as walking, squats, calf-raises, or maybe something you personally enjoy such as kickboxing moves or mock golf swings.
The Role of Essentially Fatty Acids
Inflammation of blood vessels is associated with hypertension, vasculitis, atherosclerosis, heart attack, and stroke[16]. Recognition of inflammation’s role in cardiovascular disease is a relatively recent advancement in cardiology[17]. One very important factor in systemic inflammation is the balance of essential fatty acids in the body. Omega-3 and omega-6 fatty acids, are considered “essential” because we have to consume them, as they cannot be made within humans; therefore, the ratio of essential fatty acids that we eat determines the ratio we have in our bodies[18]. They are needed as structural components of our bodies, with omega-3 fatty acids making up about 19% of brain weight for example[88]. They are also present in the cell membranes of our cells, and are used for hormone production. Omega-6 is naturally inflammatory, and omega-3 is anti-inflammatory[19]. Why would an essential nutrient be inflammatory? Well, one example of a necessary inflammatory process is when the immune system kills pathogens such as viruses and bacteria[20]. Another example is that swelling from injuries can reduce blood loss.
According to Kaur, Chugh, and Gupta (2012), about 95-99% of the population consume less than the amount of omega-3 needed to be healthy, with the average consumption falling by 80% over the past 150 years[18]. We should ideally consume close to a 1:1 ratio of omega-3 to omega-6, but the average person eats closer to a 1:16 ratio[19]. This excess level of omega-6 and relative lack of omega-3 contributes to systemic inflammation.
A major problem with modern diets is the historically unprecedented use of vegetable oils (also known as seed oils) in cooking. One reason for the unhealthy ratio of essentially fatty acids in the average modern diet is that most vegetable oils are high in omega-6 and low in, or devoid of, omega-3. Such oils include corn, safflower, cottonseed, grape seed, sesame, soybean, peanut, and sunflower, and are used in restaurants and processed foods, and sold in grocery stores with labeling marketing them as ‘healthy.’ These oils are great for burning in a diesel engine, not for eating. Historically used fats for cooking predominantly included olive oil, animal fats such as lard, beef fat, and butter, and coconut oil, although some vegetable seed oils do have a long history of use. How did we arrive at the current popularity of vegetable oils?
Creating a new market as a side-product of their innovative industrial soap production, Proctor & Gamble introduced Crisco in 1911, as a ‘healthy’ alternative to animal fat, shortly following the invention of the process for hydrogenating vegetable oils (ie turning them from liquid to solid at room temperature)[21, 32]. The danger of hydrogenated vegetable oils, stemming from their artificial trans fat content, was not widely recognized until the late 1990’s. I remember commercials in the ’90s for “I Can’t Believe It’s Not Butter,” advertising the brand-name margarine (similar to Crisco) as a supposedly healthy alternative to butter.
Trans fat is now recognized to sharply increase the risk of cardiovascular disease. Trans fats boost LDL (‘bad’ cholesterol), and decrease HDL (‘good’ cholesterol). Calling LDL and HDL ‘bad’ and ‘good,’ respectively, is an oversimplification, but let it suffice for the scope of this article. A comprehensive literature review of trans fat studies, by Ascherio et al. (2006), found a strong association between trans fats and coronary heart disease[33]. Denmark banned hydrogenated oil trans fats in foods, and decreased coronary heart disease deaths by 50% over a 20-year period[22]. A 1997 study from the New England Journal of Medicine found that women almost doubled their risk of coronary disease for every 2% of carbohydrate calories replaced by trans-fat calories[23]. However, the study’s authors found no increased risk associated with with total fats replacing carbohydrates by 5% of caloric intake, found a decreased risk by replacing carbohydrates with unsaturated fats, and also they noted poor correlation and mixed findings relating non-trans fats, including saturated fats, to health risks in previous studies. Concerning total fats, it is also notable that a 1975 study published in The American Journal of Clinical Nutrition found that Greenland Eskimos consumed a large amount of fat from seafood, but due to their high consumption of omega-3 and low consumption of omega-6, they had practically no cardiovascular disease, and had lower triglycerides, blood pressure, heart rates, and atherosclerosis, when compared to Greenland Eskimos living in Denmark, who did not significantly differ from other people living in Denmark[24].
A small amount of trans fats do occur in dairy products, because of the natural hydrogenation that occurs in stomachs of ruminant animals. More research is needed in this area, but this natural trans fat may actually be beneficial to humans[25].
As public knowledge of the dangers of trans fats from industrial hydrogenation have proliferated, marketing efforts have shifted to promote use of liquid vegetable oils, promising another ‘healthy’ alternative to supposedly dangerous butter and animal fat, and relatively expensive olive oil. Vegetable oils are called ‘refined, deodorized, bleached oils (RBD). These RBD oils are extracted with chemical solvents and heat that spoils the unstable polyunsaturated oil, so that it smells rancid, and are then bleached and deodorized to appear edible[26].
One such vegetable oil, developed by selective breeding starting in 1959, and first marketed in the US in the 1980’s, is CANOLA oil[27]. CANOLA stands for ‘Canadian Oil Low Acid.’ It is extracted from rapeseed varieties bred to be low in toxic erucic acid. Rapeseed comes from an eponymous plant in the Brassicaceae family, similar to mustard, collard greens, and broccoli. The acronym ‘Canola’ is used as a more attractive name, but it divulges a notable distinction: the toxic acid is present at a low level—it’s not absent. Erucic acid causes dangerous accumulations of fat in the heart muscle. In 2016, The European Food Safety Authority proposed lowering the maximum allowable level of erucic acid in canola oil from 5% to 2%, and approved this change in 2019[27, 28]. The US Food and Drug Administration also limits erucic acid to 2%[29]. This improvement is good news, but does not eliminate the toxin, and canola oil nevertheless should be considered unsuitable for cooking, since it is about 28% polyunsaturated fat, which is not heat stable. By contrast, olive oil contains only about 10% polyunsaturated fat.
Canola and other vegetable oils high in polyunsaturated fats absorb free radicals upon heating, and excess free radicals can cause inflammation. Omega-6 and omega-3 essential fatty acids are polyunsaturated fats. Although omega-3 is anti-inflammatory, it is not heat stable, so cooking with polyunsaturated fats, even if high in omega-3, contributes to consumption of free radicals. Free radicals are highly reactive molecules with one or more ‘extra,’ unpaired electrons; the electrons can damage all types of molecules is cells, such as proteins including DNA, and are a primary contributor to inflammation[30]. Antioxidants neutralize excess free radicals, which is why they are so crucial for health. Omega-3 fatty acids (when undamaged by heat) act as antioxidants[31, 18].
Studies have shown that supplementing diets with omega-3 fatty acids lowered the risk of heart attack and other cardiovascular death, and also reduced the thickness of carotid arteries while improving blood flow[18]. Eating more fish, flax and chia seeds, and grass-fed meats, and avoiding grain-fed meats, vegetable oils, and processed foods containing vegetable oils, can improve the ratio of omega-6 to omega-3 in our bodies[34]. A popular and effective way to improve this ratio is to take fish oil or flax seed supplements. If you take a flax supplement, look for cold-pressed flax oil, which is extracted without heat that can create free radicals and damage omega-3[35]. When selecting a fish oil supplement, avoid excessive mercury, by using oil sourced from small fish low in the food chain, such as anchovies or herring. Make sure the fish oil has a high ratio of omega-3 to omega-6, and be sure to avoid fish oil, flax oil or any other supplement or food containing polysorbate 80 (or other polysorbate), which is an emulsifier (emulsifiers dissolve oils in water; soap is an example of an emulsifier) that is harmful to the cardiovascular system, and can destroy cells by rearranging the structure of cell membranes including in red blood cells[36]. Also avoid fish oil supplements containing soy oil, which is estrogenic, and also highly likely to be from GMO Round Up-Ready soy, whole fields of which are doused in Round-Up and thereby contaminated with the herbicide[37]. “Round Up-Ready” means the soy is genetically modified (aka ‘transformed’) to be resistant to Round Up, allowing weeds to be eliminated from soy fields by blanket coverage of the fields with the dangerous chemical mixture. The ‘active’ compound in Round Up is glyphosate, which is toxic enough on its own, but as I previously highlighted in my article on covid testing, additives in pesticides can drastically increase toxicity of the ‘active’ component[38]. Much of the canola varieties grown today are likewise genetically modified to resist Round Up, giving us one more reason not to use canola oil.
The impact of essential fatty acids in healthy circulation is profound, and the modern diet contains too much omega-6, and relatively too little omega-3 fatty acids. The unhealthy ratio of essential fatty acids the average person eats contributes to systemic inflammation, including inflammation of the cardiovascular system. This ratio can be improved by avoiding vegetable oils, and by taking fish oil and flax oil supplements. Vegetable oils are pushed as ‘health foods,’ but they are really a detriment to our health, and are even worse when used for cooking. Hydrogenated vegetable oils are being phased out due to their harm to the cardiovascular system. Other harms associated with particular vegetable oils include glyphosate contamination (GMO crops), erucic acid content (canola), and estrogenic effects (soy).
Vitamin C for Collagen Synthesis
Vitamins are vital for your health, meaning they have to be consumed for survival and health. The roles of vitamins are falsely oversimplified, by commonly saying they’re each important for one thing or another; for example vitamin A for your eyes, or vitamin D for your immune system. In reality, all vitamins are important for multiple functions in your body. In accord with this rule, vitamin C serves numerous critical roles, including in cell division, enzyme function, detoxification of heavy metals, immune system activity, hormone balance, and aiding iron absorption; however, this article will focus on vitamin C’s roles as an antioxidant and in collagen production, as related to healthy circulation[39].
Interestingly, humans are amongst a small group of animals, including fruit bats and guinea pigs, that are unable to make their own vitamin C. Most animals do not need to consume vitamin C because they are able to produce it in their bodies.
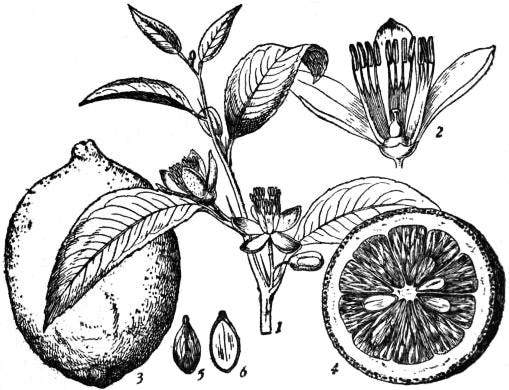
Image: Botanical drawing of lemon, Citrus limonum
Vitamin C was discovered as a result of scurvy affecting sailors. The trivial name of vitamin C is ascorbic acid, derived from the term “scorbutic,” which means ‘suffering from scurvy.’ Although ascorbic acid was not isolated until 1928, for which Albert Szent-Gorgyi was awarded the Nobel Prize, Dr. James Lind, MD (Scotland, 1716-1794), is credited with having discovered that citrus can prevent scurvy[40]. The British had vague knowledge of the anti-scorbutic effect of citrus since the 1600’s, and at least two British physicians had recommended citrus to prevent scurvy, but Lind solidified this understanding in 1747 by performing one of the first ever controlled clinical experiments in history. He divided a group of 12 scorbutic sailors into six treatment groups, and the first group—given cider—showed some improvement, while the two sailors in the fifth group, who each ate two oranges and one lemon per day for five days, showed compelling results, with one sailor having completely recovered, and the other having nearly recovered. Lind wrote his remarkably fascinating A Treatise on the Scurvy in 1753, and also developed a citrus juice concentration/preservation method for sailors to use[41, 42]. Lind expressed that his motivation for the treatise was to alleviate suffering from scurvy; he warned that some preconceived notions indoctrinated into medical students may need to be discarded to clearly perceive the disease’s cause and treatment; he also interestingly showed some frustration regarding efforts to convince healthy people to take the necessary steps to stay healthy, saying (repeated from the introduction to this article):
“It is indeed difficult to persuade some to practice, when in health, what is necessary to preserve so valuable a blessing[41].”
Health is indeed a blessing from God. This quote is pertinent today because we often tend to ignore the potential health consequences of our actions until we require medical intervention. As was true in Lind’s time, doctors don’t have all the answers, and prevention is often better than a cure. To this day, the full scope and details of vitamin C’s roles are yet to be elucidated, and remain controversial. And like all of questioning, critical, actual science—not dogmatic scientism, which to my chagrin is frequently referred to as “the science”—our current understanding is simply the best model to explain things with the available evidence, and we will never stop learning. But I digress…
Dr. Linus Pauling (1901-1994), a brilliant multidisciplinary scientist and winner of the 1954 Nobel Prize for Chemistry, noticed that the only animals that suffer from cardiovascular disease are those that cannot make vitamin C[43,44]. He also noted that researchers had found that atherosclerotic plaque deposits in arteries are not evenly distributed throughout the body, but instead are concentrated in areas close to the heart that are subjected to the highest pressure. Pauling proposed, in his 'Unified Theory of Human Cardiovascular Disease,' that plaque deposits are a repair mechanism in response to pressure-induced blood vessel damage, resulting from collagen deficiency caused by chronic vitamin C deficiency[45]. Collagen production requires vitamin C, and collagen deficiency from deprivation of vitamin C causes abnormalities in the structure of blood vessels, including abnormal endothelial cells lining the vessels, and abnormal smooth muscle cells in the vessel walls, and causes a lack of strength and elasticity of the vessels[46, 47]. Pauling recognized that animals able to produce vitamin C often make large amounts equivalent to human doses of 10,000 mg to 20,000 mg per day[45]. He proposed a therapy for atherosclerosis, consisting of 5,000-10,000 mg of vitamin C per day, and several other supplements (full list here)[44].
Human requirements for vitamin C increase under stress, such as from chronic illnesses, respiratory infections, arthritis, and gingivitis[46]. The current recommendations for daily intake of vitamin C are sufficient to prevent acute scurvy, but are insufficient to prevent subclinical manifestations of scurvy, including, as Pauling proposed, cardiovascular disease that gradually worsens over a period of years or decades[48]. Mammals that are able to produce vitamin C make quantities several orders of magnitude higher than the current recommended daily allowance (RDA), in order to stay healthy and counteract stress. Saying the RDA of 90 mg VC/day (men) and 75 mg VC/day (women) is sufficient, is analogous to saying that “cancer victims are in good health as long as the terminal signs of the disease are not evident,” as stated by researcher Irwin Stone[49, 48].
Although vitamin C levels in the bloodstream reach a maximum of about 150-220 µM from supplementation, cellular levels can be many times higher than bloodstream levels: for example, 27 times higher in lymphocyte white blood cells, and 67 times higher in neurons[50]. By my interpretation, this seems to indicate that absorption by cells throughout the body may be rapid enough to keep the bloodstream levels relatively low; in other words, as VC enters the bloodstream from the intestines, the rate at which it then leaves the bloodstream and enters cells may be fast enough to keep the bloodstream level from rising more than is observed. The low levels of VC found in blood relative to cells may also indicate that consistent supplementation or consumption of food sources of VC throughout the day is necessary to build up and maintain healthy cellular levels. I believe that the high levels of VC found in cells, and the daily production levels of mammals that can manufacture VC, show that although bloodstream concentrations of the vitamin are a valuable indication of VC status in an individual, with levels below 11.4 µM considered deficient, bloodstream concentrations may not be indicative of bodily needs[51,52]. Yet bloodstream (plasma) concentrations are the primary measure used in VC studies. Estimates of the total body pool of the vitamin vary widely, from about 1.2 g to 2.0 g, and seem too low considering known concentrations in certain cell types[42]. VC is actively transported into cells, meaning diffusion into cells is not relied upon, and VC can be moved from the lower concentrations in the blood, into cells with higher concentrations[53]. Therefore, this raises the possibility that bloodstream concentrations only drop once cellular levels are not just depleted, but severely depleted. In other words, cellular levels could be depleted before seeing any evidence in the bloodstream concentration.
Vitamin C as an Antioxidant
Free radicals are associated with DNA damage leading to cancer, and other degenerative tissue damage, and can cause inflammation of blood vessels, as discussed above in the section on essential fatty acids[50, 49]. Vitamin C acts as a redox buffer antioxidant capable of neutralizing free radicals[39]. A buffer is a substance that helps a solution (such as blood or the fluid within cells) maintain a steady pH. A well-buffered solution is able to neutralize alkalinity or acidity added to the solution, and thereby maintain pH. Although pH is commonly thought of as a measure of acidity or alkalinity, it is equally valid to see pH as a measure of electrical charge. In this view, pure water is neutral, acidity is positive charge, and alkalinity is negative charge. As a redox (reduction-oxidation) buffer antioxidant, vitamin C is able to 1: neutralize free radicals that threaten to damage tissues, such as DNA, with excess positive or negative charge, and 2: maintain the body’s pH (electrical balance), which must be kept approximately at a constant pH 7.4 (slightly alkaline/positive charge)[54].
As a horticultural scientist, I’m aware that plants must also maintain electrical equilibrium, and this causes them to, for example, take up a proton (1+ charge) of acidity from the soil when they take in a nitrate ion (plants’ preferred source of nitrogen), which carries a negative one charge. Likewise, I believe the body’s requirement to maintain electrical balance (ie maintain pH) may explain why calcium citrate is absorbed more efficiently than calcium carbonate[55]. Calcium is alkaline, and so is carbonate[56, 57]. On the other hand, citric acid (citric acid should not be confused with vitamin C), which is paired with calcium in calcium citrate, is acidic, as its name implies[58]. This electrical balance-maintaining acid-base combination in calcium citrate may explain the higher absorption of calcium from calcium citrate, when compared to calcium absorption from the base-base combination of calcium carbonate.
Some people prefer to get their vitamin C [VC] from supplements known as ‘buffered’ VC, which is VC combined with alkaline minerals such as calcium and magnesium[59]. A 2006 study by Gruenwald et al found that VC from the buffered form calcium ascorbate was tolerated significantly better than pure VC, causing less gastric upset[60]. Although there is a lack of research in this area, I suspect that not only is calcium ascorbate easier on the digestive system, it may also provide enhanced uptake of VC. If, like me, you take a pure VC supplement, I suggest taking calcium and/or magnesium or other alkaline supplements at the same time, to ease digestion and potentially enhance uptake of VC and the alkaline supplements. However, consider the maximum recommended daily doses of such supplements. The proposed upper limit for daily intake of calcium is 2,500 mg (ages 19-50) and 2,000 mg (ages 50 and up), and for magnesium it is 350 mg[61].
Although free radicals are commonly thought of as arising from stress such as excess UV rays or exposure to environmental pollutants, free radicals are actually a natural and necessary aspect of metabolism, and are used for enzyme function, signaling, and immune defense[50]. We could not live with too few or too many free radicals, and vitamin C helps maintain this balance.
In school we typically are taught that our bodies use respiration to make ATP from glucose and oxygen, and that ATP (and similarly NADPH) is the source of energy for our cells. What we are not told with the proper emphasis is that ATP and NADPH are electron donors; in other words, they carry electricity[62]. What is not emphasized is that we run on electricity! ATP and NADPH are made in our cells’ mitochondria; therefore, mitochondria are a natural site for free radical formation[62, 50, 63]. As mentioned above, neurons have high levels of vitamin C, and this is because the brain is a site of pronounced ATP production[50]. VC protects the brain from ischemic stroke by preventing it from happening, and by reducing damage caused by lack of oxygen in stroke cases[49]. VC prevents stroke by averting formation of atherosclerotic plaques and preventing damage to blood vessels, and by aiding in blood vessel dilation[49]. VC reduces damage caused by ischemic stroke by its antioxidant action, scavenging free radicals generated by oxygen deprivation in blood-deprived brain tissue[49]. A 20-year study in the United Kingdom, and a similar study in Finland, found the lowest risk of stroke in adults with the highest levels of VC consumption[64].
While overwhelming evidence shows the antioxidant character of VC, many researchers note its possible pro-oxidant effects. However, the only evidence for pro-oxidant effects is from in vitro experiments (ie ‘in glass’ tissue culture experiments in petri dishes, test tubes, etc.), and no evidence of pro-oxidant effects exists from in vivo experiments (ie in living humans)[42, 50]. Additionally, the 2020 review by Barańska et al concluded that in vitro data shows beneficial pro-oxidant effects (albeit this data may not extrapolate in vivo)[50]. In vitro data also interestingly suggests pro-oxidant activity at low doses and antioxidant activity at high doses, which if assumed to be applicable in vivo, would suggest that the higher levels that may result from supplementation would result in antioxidant activity.
Although some authors have cautioned of a risk of kidney stones and excess iron absorption from VC supplementation, The Food and Nutrition Board’s panel on dietary antioxidants and related compounds advised that in vivo data do not clearly indicate such a relationship[42]. Gerster (1997) noted that Harvard’s large-scale Prospective Health Professional Follow-Up Study found that participants in the highest intake group, who consumed more than 1,500 mg of VC per day, had a lower risk of kidney stone formation than participants with the lowest intake of VC[65]. Very large doses of VC have not been shown to have toxic or deleterious effects, and massive-dose injections into the abdomen—as an experimental cancer treatment with positive results—of 4,000 mg VC/kg of body weight, did not harm normal tissues[42, 50].
While studies examining vitamin C’s prevention of cardiovascular disease have had mixed results, with some studies showing no benefit, other studies have shown significant benefit for both sexes, and rarely have studies found a negative association. Notably, Levine et al (1996) concluded that VC reverses dysfunction of endothelium-controlled dilation of blood vessels in patients with coronary artery disease[66].
It seems that pressure from the medical establishment to remain positionally-stolid in the interest of being unbiased, and the lack of profitability from generic vitamin C, have discouraged greater enthusiasm for the vitamin in supplemental forms, and have led to promulgation of poorly-evidenced risks. Meanwhile, highly-profitable cardiovascular drugs with considerable risks are commonly prescribed. Dr. Pauling’s proposed VC-based treatment for cardiovascular disease is particularly intriguing, as it addresses underlying causation. The body’s pH/electrical balance is a subject that I suspect will receive more attention in the future, as it impacts all bodily and cellular processes, and VC likely plays a principle part in this regard. VC’s role as an antioxidant is well established, and its significance should not be underestimated.
B Vitamins in Cardiovascular Health
B vitamins are distinct individual compounds, that are water-soluble, and are grouped together because of commonalities in their characteristics, their shared natural sources, and overlapping biological roles[67]. B vitamins are known to play important roles in cardiovascular health.
Chambers et al (2000) found that randomized, double-blind supplementation with B9 (folate) and B12 (cobalamins) in patients with coronary heart disease, significantly increased flow-mediated arterial dilation compared to placebo, and concluded this is direct evidence that B vitamin supplements may reduce cardiovascular danger in people with atherosclerosis[68].
After a review of 77 papers in the medical literature related to thiamine (B1), Eshak and Arafa (2018) concluded that B1 deficiency was commonly found in patients with cardiovascular disease, and that the deficiency may be a causal factor[69]. They also suggested that patients suffering from, or at risk of, cardiovascular disease should take B1 supplements[69].
B2 (riboflavin) deficiency has been directly associated with risk factor factors for heart disease, and also indirectly associated with risk factors, by B2 deficiency interfering in metabolism of other B vitamins, including B3, B6, B9, and B12 [70]. B2 is also involved in iron metabolism, and B2 deficiency has been linked to anemia[71]. Powers et al. (2011) found that corrected B2 levels increased circulating hemoglobin[72].
As an addition to natural food sources, B vitamin supplements are popular and can help ensure adequate intakes. B vitamins including B2 are sometimes deficient even in affluent populations, indicating the potential benefit of using supplements for people with sufficient caloric intake[70]. ‘Niacin flush’ is a common sensitivity to niacin (B3) supplements and natural sources of B3 such as kombucha tea, causing red skin, itching and burning, and discomfort[73]. It may be avoided by starting at a low dose and gradually increasing dosage, by taking wax-matrix, time-released niacin, and by taking niacin in the form of inositol hexanicotinate, which is commonly referred to as “no-flush” niacin[73, 44]. Sensitivity to other B vitamins can also occur, so consult your physician and discontinue use if unusual symptoms arise. However, B vitamin supplements are often sold in surprisingly high doses, and avoiding such excessive doses can prevent side-effects[74].
Nitric Oxide: A Primary Cardiovascular Signaling Molecule
Furchgott, Ignarro, and Murad won the Nobel Prize for Physiology and Medicine in 1998 for their discoveries of nitric oxide’s [NO] roles as a key signaling molecule of the vascular system[75]. NO is a free radical that causes vasodilation, meaning it relaxes the muscles in blood vessel walls and thereby expands the vessels for freer blood flow[76]. NO has anti-atherosclerotic and anti-thrombotic (prevents mobilized plaques that obstruct vessels) properties[77]. NO prevents atherosclerosis by inhibiting LDL and related fat-protein molecules from adhering to blood vessel walls, by preventing white blood cells from congregating and combining with atherosclerotic plaques, by inhibiting platelet aggregation and adhesion, and by preventing vascular smooth muscle cells from proliferating and thickening vessel walls in the region of plaques[77, 76]. NO also promotes the growth of new blood vessels (angiogenesis) in the case of occluded vessels, thereby re-establishing blood supply and preventing tissue damage[77].
Image: Fresh beets, Beta vulgaris. Beets promote bodily production of nitric oxide (NO)
Source: Wikicommons, https://commons.wikimedia.org/wiki/File:Red_beet_(Beta_vulgaris_L.).jpg
Beet supplements that boost NO production are popular and available as tinctures, capsules, and powders. Vitamin C also plays a role in inducing the synthesis of NO, thereby increasing dilation of blood vessels[49].
NO’s importance in healthy circulation is a subject currently being studied intensively, and rightly so. Its multiple mechanisms of preventing cardiovascular disease are impressive, and testimonial evidence from users of NO-boosting products is encouraging of their beneficial effects. I occasionally eat baked beets and drink beet juice, and take beet capsules or tinctures, and can attest that I’ve experienced blood pressure-lowering effects.
Water Structure, Sunlight, and Sulfur, for Electrical Charge of RBCs, Vessels
Dr. Stephanie Seneff (of MIT) and Dr. Robert M. Davidson performed an extensive review of the medical literature, citing 335 sources, and formulated a hypothesis that novel factors affecting flowability of blood are the root cause of cardiovascular disease and sudden cardiovascular deaths[78]. These proposed novel factors affect electrical charge interactions that organize the suspension of, and shape of, red blood cells [RBCs]. Charge interactions are also hypothesized to help move RBCs through the microvasculature including the capillaries.
Strong evidence cited by the researchers suggests that surfactants (compounds that act like soap) introduced to the bloodstream interfere with the maintenance of a homogenized suspension of RBC’s, which are normally suspended in a colloidal (i.e. cloud-like) mixture with plasma[78]. A second proposed consequence of surfactants is disruption of the organized ‘structure’ of water, which is regulated by compounds including sulfates, located in the glycocalyx (gel-like layer on the surface of cells, including on endothelial cells which line the inside surface of blood vessel walls)[78]. The researches note that the majority of water in the body is tightly linked by adhesion to surfaces including the walls of vessels and the surfaces of blood cells, and they refer to this water as ‘interfacial’ water[78]. Unaffiliated but related research by Gerald Pollack, into ice formation and weather events relying on an ‘exclusion zone’ of interfacial water, reinforces the importance of water’s organizational structure[79]. Furthermore, a well known, related phenomenon in plants is avoidance of freeze damage by supercooling of water within plants. Supercooling allows water to get far below 0℃ without forming ice. A simple and amazing demonstration of supercooling, evidencing the organization of water, which can be done at home, starts by placing a bottle of purified water in the freezer, and waiting for it to get below freezing temperature[80]. The water can then be induced to instantly crystalize into ice by disturbing it, such as by flicking the bottle or by pouring it onto a surface. It’s thought that the disturbance aligns some of the water molecules into the necessary orientation to create a ‘seed’ for ice formation.
Seneff and Davidson speculate that surfactants disturbing the interfacial-water and colloidal-suspension organization of the blood can lead to a catastrophic disruption of blood flow, by causing gelatinization and coagulation of blood, and a domino-effect cascade of other biochemical events that occludes the smallest blood vessels (microvascular ischemia), leading to heart attacks, stroke, and death[78]. Such surfactants include polysorbates (aka ‘Tween’), and aluminum and mercury[78]. Polysorbate emulsifiers are found in dairy products, processed foods, dietary supplements, sunscreens, cosmetics, lotions, vaccines, and other products. Disodium phosphate is another example of an emulsifier found in dairy products and elsewhere, that like other inorganic phosphate food additives, has known dangers to the vascular system, including the calcification of blood vessels and damage to the endothelial lining of blood vessels[81]. Emulsifiers such as polysorbates and phosphates, as mentioned in the above section on essential fatty acids, are surfactants used to dissolve oils into water-based solutions. Aluminum and mercury also have surfactant effects, and are included as additives in vaccines[78]. Aluminum is also present in anti-perspirant deodorants and sunscreens.
The other hypothetical (albeit supported by compelling, indirect evidence) aspect of the Dr. Seneff’s research is the idea that sulfur compounds are used by the human body to harvest electrical energy from sunlight, and this energy is used to propel RBCs through the smallest blood vessels. If this idea seems radical to you, before I explain, consider that humans use sunlight to produce vitamin D.
Albeit yet to be proven experimentally, Seneff and colleagues assert that the enzyme used to make NO in blood vessels is a dual-purpose enzyme and is also used to produce sulfate from dietary sources of sulfur, in the presence of sunlight[82]. In their model, red blood cells [RBCs] obtain negative charge from photons (‘light particles’) from the sun, as they move through veins near the skin’s surface, such as the veins on the back of our hands, and store the negative charge in sulfate molecules attached to the RBCs[83]. When the RBCs are pumped from the heart and reach the smallest arteries and capillaries, they shed some (but not all) of the negative charge into the lining of the capillaries[84]. This provides the capillary walls with negative charge[84]. Because negative charge repels other negative charge, this helps RBCs move through tiny capillaries by repulsion that keeps them from sticking to the capillary walls[84]. Further propelling RBCs through the capillaries is the fact that RBCs take on CO2 (carbon dioxide) from cells and carry it away for expulsion from the lungs. CO2 forms carbonic acid in the veins[85]. As explained above, in the section on Vitamin C as an antioxidant, acid has a positive charge. The relatively positive charge from carbonic acid in the veins attracts the negatively charged RBCs and pulls them through the capillaries[84]. Seneff’s hypothesis also implicates interactions between sulfur and cholesterol as important in maintaining the homogenous suspension of RBCs, maintaining cell membrane integrity, and repairing arterial damage[82].
In one independent experiment indirectly supporting the proposed novel role of sulfur in preventing atherosclerosis, researchers who induced atherosclerosis-like disease in Cebus monkeys by feeding them a high-fat, high-cholesterol, high choline diet, were able to prevent the condition by concurrently feeding them sulfur-containing amino acids[83]. Another telling corroboration is that garlic consumption has been associated with prevention of atherosclerosis, and it’s possible that sulfur in garlic is the preventative factor[83]. An additional role of sulfate is binding with positively charged toxins such as aluminum and mercury, thereby helping the kidneys remove them from the body[78]. Furthermore, the fact that sulfur is the third most plentiful mineral in the body, clearly points toward the importance of dietary sulfur, and makes indications of sulfur’s role in heart health unsurprising[86].
These findings indicate that eating a good supply of sulfur rich foods, and getting plenty of sun, could be important factors in healthy blood circulation. Foods rich in sulfur include brassicas, garlic, onions, meats, legumes, and whole grains[86]. Interestingly, the sulfur source in whole grains is thiamine (vitamin B1)[86], so this brings to light the prospect that the cardiovascular benefits of B1 may arise at least in part from sulfur. Although the proposed disruption of structured water organization, as a primary cause of catastrophic cardiovascular events, is a novel implication for the effects of emulsifiers/surfactants, previously established dangers of emulsifiers to cardiovascular health are alone enough reason to avoid them. This new idea adds yet more impetus to recognize the danger, and deserves further research.
Conclusions
Hopefully this synthesis of factors involved in healthy blood circulation will help people maintain and improve their cardiovascular health, and will encourage further research and the development of new perspectives. Hydration, frequent movement throughout the day along with elevating the legs and daily exercise, the ratio of omega-3 to omega-6 consumed from various sources, sufficient vitamin C and B vitamin intake, nitric oxide production, dietary sulfur, adequate sunlight, and avoidance of emulsifiers/surfactants, are all factors that should be considered in the interest of cardiovascular health.
References
[1] Song, S.H., Kim, J.H., Lee, J.H. et al. (2017) Elevated blood viscosity is associated with cerebral small vessel disease in patients with acute ischemic stroke. BMC Neurol 17, 20 (2017). https://doi.org/10.1186/s12883-017-0808-3
[2] Sloop G D, De Mast Q, Pop G, et al. (February 24, 2020) The Role of Blood Viscosity in Infectious Diseases. Cureus 12(2): e7090. doi:10.7759/cureus.7090 https://www.cureus.com/articles/27906-the-role-of-blood-viscosity-in-infectious-diseases#!/
[3] Holsworth Jr, R. E., Cho, Y. I., & Weidman, J. (2013). Effect of hydration on whole blood viscosity in firefighters. Altern Ther Health Med, 19(4), 44-49. https://denverfireonline.com/wp-content/uploads/2014/08/147874480-Effect-of-Hydration-on-Whole-Blood-Viscosity-in-Firefighters-2.pdf
[4] Cardiovascular diseases (CVDs) 11 June 2021. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
[5] Weideman, M. P. (1963) Dimensions of Blood Vessels from Distributing Artery to Collecting Vein. Circulation Research 1963-04-01 12(4): 375-378 https://www.ahajournals.org/doi/epdf/10.1161/01.RES.12.4.375
[6] Suadicani P, Hannerz H, Bach E, Gyntelberg F. (2012) Jobs encompassing prolonged sitting in cramped positions and risk of venous thromboembolism: cohort study. JRSM Short Rep. 2012 Feb;3(2):8. doi: 10.1258/shorts.2011.011121. Epub 2012 Feb 14. PMID: 22393469; PMCID: PMC3291423. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3291423/
[7] Aviroop Biswas, Paul I. Oh, Guy E. Faulkner, et al. (2015) Sedentary Time and Its Association With Risk for Disease Incidence, Mortality, and Hospitalization in Adults: A Systematic Review and Meta-analysis. Ann Intern Med. 2015;162:123-132. [Epub 20 January 2015]. doi:10.7326/M14-1651 https://www.acpjournals.org/doi/full/10.7326/M14-1651
[8] Michael Joseph Blaha, M.D., M.P.H. Why Exercise Isn't Enough to Keep Your Heart Healthy. https://www.hopkinsmedicine.org/health/wellness-and-prevention/why-exercise-isnt-enough-to-keep-your-heart-healthy
[9] Carmen Chai. Sitting all day at work? Get up every 30 minutes to cut your risk of death https://globalnews.ca/news/3740438/sitting-all-day-at-work-get-up-every-30-minutes-to-cut-your-risk-of-death/
[10] Diaz, K. M. et al. (2017). Patterns of Sedentary Behavior and Mortality in U.S. Middle-Aged and Older Adults. Annals of Internal Medicine. 2017; 167, 7: 465-475 https://doi.org/10.7326/M17-0212 https://www.acpjournals.org/doi/full/10.7326/M17-0212
[11] Antle DM, Cormier L, Findlay M, Miller LL, Côté JN. (2018) Lower limb blood flow and mean arterial pressure during standing and seated work: Implications for workplace posture recommendations. Prev Med Rep. 2018 Mar 5;10:117-122. doi: 10.1016/j.pmedr.2018.02.016. PMID: 29850397; PMCID: PMC5966524. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5966524/
[12] UAMS Health. March 8, 2019. Can Standing Up Straight for a Long Period Cause Fainting? https://uamshealth.com/medical-myths/can-standing-up-straight-for-a-long-period-cause-fainting/
[13] Bell, A. M. (2021) What Are the Benefits of Elevating Your Legs? Healthline. https://www.healthline.com/health/elevating-legs
[14] Elmagd, M. A. (2016) Benefits, need and importance of daily exercise. International Journal of Physical Education, Sports and Health 2016; 3(5): 22-27 https://www.kheljournal.com/archives/2016/vol3issue5/PartA/3-4-55-201.pdf
[15] Balady, G. J. et al. (2000) Resistance Exercise in Individuals With and Without Cardiovascular Disease. Circulation. 2000; 101:828–833 https://doi.org/10.1161/01.CIR.101.7.828
[16] Sorriento D, Iaccarino G. (2019) Inflammation and Cardiovascular Diseases: The Most Recent Findings. Int J Mol Sci. 2019 Aug 9;20(16):3879. doi: 10.3390/ijms20163879. PMID: 31395800; PMCID: PMC6719998. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6719998/
[17] Tuder, R. M. and Voelkel, N. F. (1998) Pulmonary Hypertension and Inflammation. J Lab Clin Med 1998;132:16-24. https://www.sciencedirect.com/sdfe/pdf/download/eid/1-s2.0-S0022214398900208/first-page-pdf
[18] Kaur N, Chugh V, Gupta AK. (2014) Essential fatty acids as functional components of foods- a review. J Food Sci Technol. 2014 Oct;51(10):2289-303. doi: 10.1007/s13197-012-0677-0. Epub 2012 Mar 21. PMID: 25328170; PMCID: PMC4190204. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4190204/
[19] Gunnars, K. (2023) How to Optimize Your Omega-6 to Omega-3 Ratio. Healthline https://www.healthline.com/nutrition/optimize-omega-6-omega-3-ratio#TOC_TITLE_HDR_2
[20] Chen L, Deng H, Cui H, Fang J, Zuo Z, Deng J, Li Y, Wang X, Zhao L. (2017) Inflammatory responses and inflammation-associated diseases in organs. Oncotarget. 2017 Dec 14;9(6):7204-7218. doi: 10.18632/oncotarget.23208. PMID: 29467962; PMCID: PMC5805548. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5805548/
[21] Jones, M. and Cirino, C. Under the Radar: The 100-plus Year History of Vegetable Oils. Your Health Forum. https://yourhealthforumbydrcirino.org/2020/09/08/5873/
[22] Iqbal, M. P. (2014) Trans fatty acids - A risk factor for cardiovascular disease. Pak J Med Sci. 2014 Jan;30(1):194-7. doi: 10.12669/pjms.301.4525. PMID: 24639860; PMCID: PMC3955571.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3955571/
[23] Colditz, G. A. et al (1997) Dietary Fat Intake and the Risk of Coronary Heart Disease in Women. New England Journal of Medicine. 1997; 337:1491-1499 DOI: 10.1056/NEJM199711203372102 https://www.nejm.org/doi/10.1056/NEJM199711203372102?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200www.ncbi.nlm.nih.gov
[24] Dyerberg J, Bang HO, Hjorne N. (1975) Fatty acid composition of the plasma lipids in Greenland Eskimos. Am J Clin Nutr. 1975 Sep;28(9):958-66. doi: 10.1093/ajcn/28.9.958. PMID: 1163480. https://pubmed.ncbi.nlm.nih.gov/1163480/
[25] Mendis S, Cruz-Hernandez C, Ratnayake WM. (2008) Fatty acid profile of Canadian dairy products with special attention to the trans-octadecenoic acid and conjugated linoleic acid isomers. J AOAC Int. 2008 Jul-Aug;91(4):811-9. PMID: 18727541. https://pubmed.ncbi.nlm.nih.gov/18727541/
[26] Kresser, C. (2019) How Industrial Seed Oils Are Making Us Sick. https://chriskresser.com/how-industrial-seed-oils-are-making-us-sick/
[27] Darwisch, V., Lehnert, K., and Vetter, W. (2020) Erucic acid in Brassicaceae and salmon – An evaluation of the new proposed limits of erucic acid in food. NFS Journal. June 2020, (19): 9-15 https://www.sciencedirect.com/science/article/pii/S235236462030002X
[28] COMMISSION REGULATION (EU) 2019/1870. Official Journal of the European Union https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32019R1870&rid=1
[29] Code of Federal Regulations Title 21. US Food and Drug Administration. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=184.1555
[30] Bagchi, K. and Puri, S. (1998) Free radicals and antioxidants in health and disease. Eastern Mediterranean Health Journal (4) 2: 350-360. https://apps.who.int/iris/bitstream/handle/10665/118217/emhj_1998_4_2_350_360.pdf?sequence=1
[31] Akbari, A. et al. (2019) Omega-3 fatty acids supplementation and oxidative stress parameters: A systematic review and meta-analysis of clinical trials. Pharmacological Research. 2019, 149. https://doi.org/10.1016/j.phrs.2019.104462. https://www.sciencedirect.com/science/article/abs/pii/S1043661819311910
[32] Ramsey, D. and Graham, T. (2012) How Vegetable Oils Replaced Animal Fats in the American Diet. The Atlantic. https://www.theatlantic.com/health/archive/2012/04/how-vegetable-oils-replaced-animal-fats-in-the-american-diet/256155/
[33] Ascherio, et al. (2006) Trans fatty acids and cardiovascular disease. New England Journal of Medicine. 2006 Apr 13; 354(15):1601-13. doi: 10.1056/NEJMra054035. https://pubmed.ncbi.nlm.nih.gov/16611951/
[34] Fatty acid ratio in food. Wikipedia. https://en.wikipedia.org/wiki/Fatty_acid_ratio_in_food
[35] Anastasia, S. (2023) What is Cold Pressed Flaxseed Oil?. The Health Board https://www.thehealthboard.com/what-is-cold-pressed-flaxseed-oil.htm
[36] Information for the package leaflet regarding polysorbates used as excipients in medicinal products for human use. (2018) European Medicines Agency. https://www.ema.europa.eu/en/documents/scientific-guideline/draft-information-package-leaflet-regarding-polysorbates-used-excipients-medicinal-products-human_en.pdf
[37] elSattar ElBaltran, S. A. (2001) Studies on the oestrogenic activity of soybean oil on albino rats. Boll Chim Farm. 2001 Mar-Apr;140(2):119-24. PMID: 11417387. https://pubmed.ncbi.nlm.nih.gov/11417387/
[38] Bender, J. (2023) Testing Society’s Sensibilities: Harmful Covid Tests. The Bender Observatory.
[39] Pehlivan, F. E. (2017) Vitamin C: An Antioxidant Agent. https://books.google.com/books?hl=en&lr=&id=-PyPDwAAQBAJ&oi=fnd&pg=PA23&dq=vitamin+c+as+a+biological+buffer+&ots=rQefzZQjWy&sig=DgcMt2VYmY8iXaoYQx3AaBsqgjM#v=onepage&q=vitamin%20c%20as%20a%20biological%20buffer&f=false
[40] James Lind. Wikipedia. https://en.wikipedia.org/wiki/James_Lind
[41] Lind, J. (1753) A Treatise on the Scurvy. London. https://books.google.com/books?hl=en&lr=&id=oP1UEXWU7fsC&oi=fnd&pg=PR1&ots=sqO4jY7t2M&sig=uWq84rWLmcosbt43IIpEfDI9ujk#v=onepage&q&f=false
[42] Naidu, K.A. (2003) Vitamin C in human health and disease is still a mystery? An overview. Nutrition Journal 2, 7 (2003). https://doi.org/10.1186/1475-2891-2-7 https://link.springer.com/article/10.1186/1475-2891-2-7
[43] Linus Pauling—Biographical. NobelPrize.org. Nobel Prize Outreach AB 2023. https://www.nobelprize.org/prizes/chemistry/1954/pauling/facts/
[44] English, J, and Cass, H. (2013) Linus Pauling’s Unified Theory of Human Cardiovascular Disease. Nutrition Review. https://nutritionreview.org/2013/04/collagen-connection/
[45] Rath, M. and Pauling, L. (1992) A Unified Theory of Human Cardiovascular Disease Leading the Way to the Abolition of This Disease as a Cause for Human Mortality. Journal of Orthomolecular Medicine. 1992 (7)1: 5-12. http://orthomolecular.org/library/jom/1992/pdf/1992-v07n01-p005.pdf
[46] Abdullah, M., Jamil, R. T., and Attia, F. N. (2022) Vitamin C (Ascorbic Acid). NIH National Library of Medicine, National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK499877/
[47] Mahmoodian, F. and Peterkofsky, B. (1999) Vitamin C Deficiency in Guinea Pigs Differentially Affects the Expression of Type IV Collagen, Laminin, and Elastin in Blood Vessels, The Journal of Nutrition, Volume 129, Issue 1, January 1999, Pages 83–91, https://doi.org/10.1093/jn/129.1.83 https://academic.oup.com/jn/article/129/1/83/4723241
[48] Stone, I. (1978) Eight Decades of Scurvy: The Case History of a Misleading Dietary Hypothesis. Presentation at Annual Meeting of the Orthomolecular Medical Society. https://www.seanet.com/~alexs/ascorbate/197x/stone-i-orthomol_psych-1979-v8-n2-p58.htm
[49] Tang, X., Liu, H., Xiao, Y., Wu, L., Shu, P. (2022) Vitamin C Intake and Ischemic Stroke. Frontiers in Nutrition. 2022 Jul 14; 9:935991. doi: 10.3389/fnut.2022.935991. PMID: 35911106; PMCID: PMC9330473. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9330473/
[50] Kaźmierczak-Barańska, J., Boguszewska, K., Adamus-Grabicka, A., Karwowski, B. T. (2020) Two Faces of Vitamin C-Antioxidative and Pro-Oxidative Agent. Nutrients. 2020 May 21;12(5):1501. doi: 10.3390/nu12051501. PMID: 32455696; PMCID: PMC7285147. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7285147/
[51] Maxfield, L. and Crane, J. S. (2022) Vitamin C Deficiency. NIH National Library of Medicine, National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK493187/
[52] Jacob, R. A. (1990) Assessment of Human Vitamin C Status, The Journal of Nutrition, Volume 120, Issue suppl_11, November 1990, Pages 1480–1485, https://doi.org/10.1093/jn/120.suppl_11.1480 https://academic.oup.com/jn/article-abstract/120/suppl_11/1480/4738628
[53] (2021) Vitamin C—Fact Sheet for Health Professionals. National Institutes of Health, Office of Dietary Supplements. https://ods.od.nih.gov/factsheets/VitaminC-HealthProfessional/
[54] Hopkins, E., Sanvictores, T., and Sharma S. (2022) Physiology, Acid Base Balance. NIH National Library of Medicine, National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/books/NBK507807/
[55] Adams-Huet, B. et al. (1999) Meta-analysis of Calcium Bioavailability: A Comparison of Calcium Citrate with Calcium Carbonate. American Journal of Therapeutics 6(6):p 313-322, November 1999. https://journals.lww.com/americantherapeutics/abstract/1999/11000/meta_analysis_of_calcium_bioavailability__a.5.aspx
[56] (2021) The alkaline diet. Royal Osteoporosis Society. https://theros.org.uk/information-and-support/bone-health/nutrition-for-bones/are-there-any-foods-i-should-avoid/the-alkaline-diet/
[57] (2021) Carbonates. LibreTexts Chemistry. https://chem.libretexts.org/Bookshelves/Inorganic_Chemistry/Supplemental_Modules_and_Websites_(Inorganic_Chemistry)/Descriptive_Chemistry/Main_Group_Reactions/Compounds/Carbonates
[58] Bratskeir, K. (2021) Citric Acid vs. Ascorbic Acid: Which Is Healthier? Livestrong. https://www.livestrong.com/article/164362-difference-between-citric-acid-and-ascorbic-acid/
[59] Bartholomew, R. (2022) Confused About The Different Types of Vitamin C? Nutri Advanced. https://www.nutriadvanced.co.uk/news/confused-about-the-different-types-of-vitamin-c/
[60] Gruenwald, J., Graubaum, H. J., Busch, R., et al. (2006) Safety and tolerance of Ester-C® compared with regular ascorbic acid. Advances in Therapy. 23, 171–178 (2006). https://doi.org/10.1007/BF02850358 https://link.springer.com/article/10.1007/BF02850358
[61] (2023) Vitamin C > Supplemental Forms. Oregon State University, Linus Pauling Institute, Micronutrient Information Center. https://lpi.oregonstate.edu/mic/vitamins/vitamin-C/supplemental-forms {This link leads to a website provided by the Linus Pauling Institute at Oregon State University. Joe Bender is not affiliated or endorsed by the Linus Pauling Institute or Oregon State University.}
[62] Zhu J., Schwörer S., Berisa M., Kyung Y.J., Ryu K. W., Yi J., Jiang X., Cross J. R, Thompson C. B. (2021) Mitochondrial NADP(H) generation is essential for proline biosynthesis. Science. 2021 May 28;372(6545):968-972. doi: 10.1126/science.abd5491. Epub 2021 Apr 22. PMID: 33888598; PMCID: PMC8241437. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8241437/
[63] Milner, J. A. New Insights into the Mechanism of Action of Antioxidants. National Cancer Institute, Bethesda Maryland. https://ods.od.nih.gov/pubs/conferences/ada2002/Milner_abstract.html
[64] Gale C. R., Martyn C. N., Winter P. D., and Cooper C. (1995) Vitamin C and risk of death from stroke and coronary heart disease in cohort of elderly people. BMJ. 1995 Jun 17;310(6994):1563-6. doi: 10.1136/bmj.310.6994.1563. PMID: 7787644; PMCID: PMC2549941.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2549941/
[65] Gerster H. (1997) No Contribution of Ascorbic Acid to Renal Calcium Oxalate Stones. Ann Nutr Metab 1997; 41: 269–282 https://doi.org/10.1159/000177954
[66] Levine, et al. (1996) Ascorbic acid reverses endothelial vasomotor dysfunction in patients with coronary artery disease. Circulation. 1996 Mar 15; 93(6): 1107-13. https://pubmed.ncbi.nlm.nih.gov/8653830/
[67] Vitamin B Complex. Britannica.com https://www.britannica.com/science/vitamin-B-complex
[68] Chambers et al. (2000) Improved Vascular Endothelial Function After Oral B Vitamins: An Effect Mediated Through Reduced Concentrations of Free Plasma Homocysteine. Circulation. 2000; 102: 2479–2483 https://www.ahajournals.org/doi/full/10.1161/01.CIR.102.20.2479
[69] Ehak E. S., and Arafa, A. E. (2018) Thiamine deficiency and cardiovascular disorders. Nutrition, Metabolism, and Cardiovascular Diseases. October 2018 (28)10: 965-972. https://www.sciencedirect.com/science/article/abs/pii/S0939475318302011
[70] Powers, H. J. (2003) Riboflavin (vitamin B-2) and health The American Journal of Clinical Nutrition. (77) 6, June 2003, Pages 1352–1360, https://academic.oup.com/ajcn/article/77/6/1352/4689829
[71] (2022) Riboflavin. Oregon State University, Linus Pauling Institute, Micronutrient Information Center. https://lpi.oregonstate.edu/mic/vitamins/riboflavin#reference18
{This link leads to a website provided by the Linus Pauling Institute at Oregon State University. Joe Bender is not affiliated or endorsed by the Linus Pauling Institute or Oregon State University.}
[72] Powers, H. J. et al. (2011) Correcting a marginal riboflavin deficiency improves hematologic status in young women in the United Kingdom (RIBOFEM). American Journal of Clinical Nutrition. 2011 93(6): 1274-84 https://pubmed.ncbi.nlm.nih.gov/21525198/
[73] Pierce, J. J. (2023) Niacin - How to Beat the Flush. Ageless Forever Anti-Aging News Blog. https://www.agelessforever.net/anti-aging-news-blog/niacin-how-to-beat-the-flush
[74] Weil, A. (2019) Can Any B Vitamins Be Harmful? drweil.com. https://www.drweil.com/vitamins-supplements-herbs/vitamins/can-any-b-vitamins-be-harmful/
[75] (2023) The Nobel Prize in Physiology or Medicine 1998. nobelprize.org https://www.nobelprize.org/prizes/medicine/1998/summary/
[76] Ignarro, L. J. (2002) Nitric Oxide as a Unique Signaling Molecule in the Vascular System: A Historical Overview. Journal of Physiology and Pharmacology. 2002, (53) 4: 503-514 https://www.jpp.krakow.pl/journal/archive/12_02/pdf/503_12_02_article.pdf
[77] Naseem, K. M. (2005) The role of nitric oxide in cardiovascular diseases. Molecular Aspects of Medicine 2005, 26: 33-65 https://scholar.google.com/scholar?cluster=17760365513968273903&hl=en&as_sdt=0,10
[78] Davidson, R. M. and Seneff, S. (2012) The Initial Common Pathway of Inflammation, Disease, and Sudden Death. Entropy 2012, 14(8): 1399-1442 https://www.mdpi.com/1099-4300/14/8/1399
[79] Pollack, G. (2017) Weather and EZ Water -- An Intimate Role of Separated Charge. Thunderbolts Project. EU2017. youtube.com
[80] Misterseng (2011) Supercooled Water. Misterseng. youtube.com
[81] Ritz, E., Hahn, K., Ketteler, M., Kuhlmann, M. K., Mann, J. (2012) Phosphate additives in food--a health risk. Dtsch Arztebl Int. 2012 Jan; 109(4): 49-55. doi: 10.3238/arztebl.2012.0049.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3278747/
[82] Seneff, S., Lauritzen, A., Davidson, R., Lentz-Maurino, L. (2012) Is Endothelial Nitric Oxide Synthase a Moonlighting Protein Whose Day Job is Cholesterol Sulfate Synthesis? Implications for Cholesterol Transport, Diabetes and Cardiovascular Disease. Entropy. 2012, 14(12): 2492-2530 https://www.mdpi.com/1099-4300/14/12/2492
[83] Seneff, S., Davidson, R. M., Lauritzen, A., Samsel, A., Wainwright, G. (2015) A novel hypothesis for atherosclerosis as a cholesterol sulfate deficiency syndrome. Theor Biol Med Model. 2015 May 27;12:9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4456713/
[84] Seneff, S. (2016) The Mineral Power for Your Body’s Electrical Supply. TEDx Talks. youtube.com
[85] Doyle, J. and Cooper, J. S. (2022) Physiology, Carbon Dioxide Transport. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK532988/
[86] Mikstas, C. (2022) Foods High in Sulfur. Nourish by WebMD. https://www.webmd.com/diet/foods-high-in-sulfur
[87] Wang, H. and Peng, D. (2011) New insights into the mechanism of low high-density lipoprotein cholesterol in obesity. Lipids in Health and Disease. 2011, 10, article 176. https://link.springer.com/article/10.1186/1476-511x-10-176
[88] Alawi, I. A. et al. (2022) Effects of Omega-3 Polyunsaturated Fatty Acids on Brain Functions: A Systematic Review. Cureus. 2022 Oct 9; 14(10): e30091. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9641984/









Shared to my Twitter!
I just had an epiphany related to one of the subjects in this article, when I got done with a set of lunges: the reason you need to keep moving after strenuous exercise, to catch your breath, and to ‘cool down,’ is because the one-way valves in the veins are responsible for moving the blood back to the heart and lungs. Therefore, when you stop moving after strenuous exercise, you create back-pressure in the veins, because they need to be squeezed by the muscles to move the blood. That must be why your heart beats harder and you get more out of breath when you suddenly stop moving.